What is a Digital Hub in 2023?
Deciphering the different "technology-first” and “technology-enabled” patient support programs.
The healthcare space is adopting and even requiring the digital processes that organizations have been driving the industry toward for over a decade. Regulators continue to emphasize innovation in healthcare, especially digital requirements for e-prescriptions, e-prior authorizations (e-PAs), and other technology-first methods.
The Centers for Medicare and Medicaid Services (CMS) continues to advance its interoperability goals and address process challenges related to e-prescribing and PAs. Proposed rule CMS-0057-P would require impacted payers to improve the electronic exchange of healthcare data and streamline PA processes.
Additionally, CMS continues to implement a provision of the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities (SUPPORT) Act that requires e-prescribing of controlled substances under Medicare Part D. Further, a recent Biden Administration proposal would implement e-PAs for several government insurer plans by 2026, as well as require payers and states to streamline PA processes and improve the electronic exchange of data. It also contains incentives for hospitals and physicians to adopt e-PAs.
While these regulatory changes will force many in the industry to adopt digital methods, the specialty pharmaceutical space may never fully transition to digital-only processes. Some may argue that the level of human intervention may always be needed, due to the complex nature of specialty product support. However, technology advancements within the space demonstrate that specialty is ready to embrace technology-first programs, or digital hubs. As noted ahead, the definition of a digital hub varies greatly by stakeholder.
Some may think a digital hub is:
- A collection of technology-enabled solutions.
- Automation when possible.
- Electronic solutions available via web, app, etc.
- Human intervention in the backend.
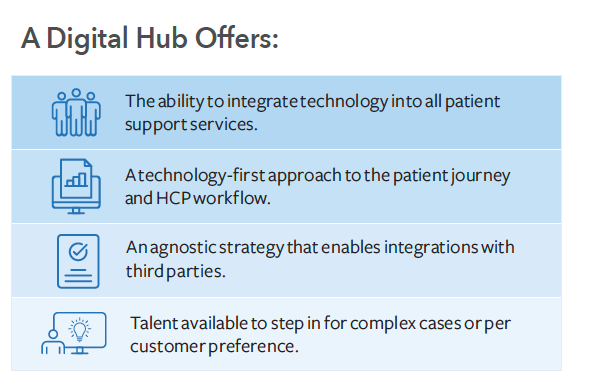
But what a digital hub actually provides is much more specific (see graphic below). The source of confusion over the definition of a digital hub can be attributed to the uncertainty between “technology-first” and “technology-enabled” patient support programs. The first step to understanding a digital hub in 2023 is to identify how these two types of programs differ.
Understanding technology-first and technology-enabled solutions
Many patient support programs deploy technology-enabled solutions in some capacity, like electronic benefit verification (e-BV) or digitized enrollment. However, leveraging technology-enabled solutions does not mean the program is a technology-first program. The difference lies in the ability to automate the process with technology, versus relying on human intervention in the backend to prop it up.
For example, some patient support providers generate electronic benefit coverage via a combination of e-BV and phone calls to the payer, whereas technology-first approaches leverage direct connectivity with payers/pharmacy benefit managers (PBMs) to return comprehensive patient coverage results in real-time. Some providers utilize digital forms for PA completion. Technology-first PAs return the appropriate patient plan- and product-specific PA question set for completion and submission to the payer/PBM, with decisions returned in minutes.
A digital hub provider possesses two qualities:
- The ability to integrate technology into all patient support services, fully automating the process, versus relying on human intervention to prop up technology.
- A strategic choice to deliver services with a technology-first approach. This means every step of the patient journey that can be completed in an electronic, automated fashion begins and ends with technology.
Patient support providers that can deliver a digital hub must have advanced, interoperable technology, as well as an agnostic stance and willingness to integrate with all parties necessary to facilitate technology-first patient support.
Which products benefit from a digital hub?
- Products that benefit most from a digital hub typically have some of the following characteristics:
- Pharmacy benefit product at a stage in its product lifecycle in which most processes can be digital and automated.
- Low wholesale acquisition cost (WAC) product unable to afford high-touch, full-time equivalent (FTE)-enabled specialty services or product approaching the loss of exclusivity (LOE) cliff.
- Technology-savvy HCP population that is familiar with specialty drug processes.
- Highly motivated, technology-savvy, and cognitively and physically able patient/caregiver population.
- A payer mix of payers/PBMs with electronic capabilities.
- Formulary position that does not require significant step edits and PA hurdles.
These products require little to no human intervention to maintain prescription journey momentum. Services can be completed in an automated fashion due to electronic connectivity and available data. Further, data required to make informed decisions, such as patient coverage information and PA requirements, can be returned with high accuracy through integrations, or direct connectivity, with the source.
It's important to note that the technology is only as good as the design. Digital hub program effectiveness depends on deploying the right technology at the right time and through the right delivery method. It’s critical that the digital hub vendor knows when and where to incorporate technology and talent not only throughout the product’s current therapy journey, but also as processes evolve along the drug's lifecycle.
Jan Nielsen

For example, a high-volume, mid-lifecycle pharmacy benefit product with short PA approval periods would benefit from a technology-first (digital hub) approach, while a first-to-market, buy-and-bill product would need talent-enabled support at launch. However, a strong patient support program vendor supporting this high-volume pharmacy benefit product would likely have implemented tech- and talent-enabled support at launch to support HCPs with navigating payer hurdles and to drive perceived access. Talent would have also been leveraged to improve payer coverage by deploying payer-targeted product demand and clinical effectiveness call campaigns, and to evaluate when the program was ready to incorporate additional technology-first solutions.
How digital hubs impact patient and HCP experiences
Today, more than half of HCPs under the age of 55 experience emotional distress and burnout in some part, due to the administrative burdens they face to ensure patient access. This realization underscores the need for digital hubs to support HCPs with simplified, automated processes. For example, digital hubs can incorporate a digital intake process that enables triggered e-support services at the point of e-prescription intake from the electronic health record/electronic medical record (EHR/EMR). This process automates and accelerates the therapy initiation process, while meeting HCPs where they are.
Digital hubs can support patients with managing their healthcare too, as many of today’s patients are familiar with digital processes. A recent survey reported that 80% of respondents have used telemedicine within their lifetime, and it's now the preferred channel for receiving prescriptions and care for some conditions. To meet patients where they are, digital hubs can incorporate omnichannel strategies, such as branded engagement websites, chatbots, and automated communications like text and email. However, these strategies must be designed and deployed in the right way for the product. A stratified, omnichannel approach based on patient segmentation yields the best results, as patients can self-serve, engage with the brand through a variety of channels and do so at their convenience.
Further, digital hubs should stratify patient populations based on adherence risk to deliver tailored technology-first and talent-enabled adherence solutions based on the patient’s risk profile and communication preferences.
HCP segmentation is needed for a successful program, too. It is essential for digital hubs to not only stratify HCP populations to meet them in their workflow, but also to identify which offices require additional support. For example, a PA denial due to a missing letter of medical necessity (LMN) for a less-technology savvy office would trigger a different follow-up task than a technology-savvy office that receives a PA denial for the same reason. The first office would receive a triggered fax containing the appropriate template LMN. The second office would receive a triggered email containing a tokenized hyperlink to complete the LMN/e-appeal.
Delivering differentiated experiences with a digital hub
Digital hubs can create tailored technology-first experiences for program stakeholders that differentiate the program in a competitive market. To remain competitive, program design must evolve with the product lifecycle, HCP technology adoption, and patient life stage/disease progression. Let’s review a few examples.
Example one
- Technology-enabled solution: Electronic benefit coverage results generated via e-eligibility or test claims.
- What a technology-first approach would look like: A solution that delivers comprehensive electronic benefit coverage results generated via direct connectivity with payers/PBMs and other data sources.
- How this technology-first approach differentiates a program: Provides accurate and comprehensive coverage results in under 15 seconds.
Example two
- Technology-enabled solution: Digital presentation of a PA form submitted to the payer/PBM through e-fax.
- What a technology-first approach would look like: An end-to-end e-PA solution that generates the digital product- and patient plan-specific PA question set, facilitates real-time submission to the payer/PBM through direct connectivity, and returns PA decisions within minutes through this same connectivity.
- How this technology-first approach differentiates a program: Enables real-time e-PA generation and submission directly to the payer/PBM to accelerate the process and create informed decisions.
Example three
- Technology-enabled solution: Virtual clinical visits with online appointment scheduling that are manually managed by call center agents on the backend.
- What a technology-first approach would look like: A clinical solution that integrates with the customer relationship management (CRM), providing automated appointment scheduling and reporting, as well as a secure channel for virtual visits.
- How this technology-first approach differentiates a program: Facilitates a full view of the patient case while delivering true technology-first patient support.
The key to a digital hub program that delivers differentiated patient and HCP experiences is the right balance of tech plus talent. By selecting a partner that implements a tailored, technology-first approach, supported by human know-how when appropriate, one can provide a digital experience for your program that increases patient uptake, facilitates greater visibility, and improves treatment outcomes.
About the Author
Jan Nielsen is Patient Solutions Division President at AssistRx.