Patient Hubs in an Omnichannel World
How personalized interventions can help boost the omnichannel experience for patient hubs—and drive engagement and impact adherence in outcomes.
Patient hubs are the backbone of any pharmacutical company’s specialty medication commercialization strategy. They do a great job of getting the right patients to the specialty pharmacy for dispensing. However, there are still gaps that hubs have not been able to fulfill, whether on the data and analytics side or understanding the patient better and customizing interventions at the right time and in the right channel. This article will focus on what patient hubs do today, and how we can improve the omnichannel experience for patients across the hub.
A patient hub is a one-stop shop connecting patients directly to special medication manufacturers, physicians, and payers, as shown in Figure 1 below. The primary task of the patient hub is to enhance engagement by reducing the barriers of affordability and access so that patients are more adherent to their treatments and have better outcomes.
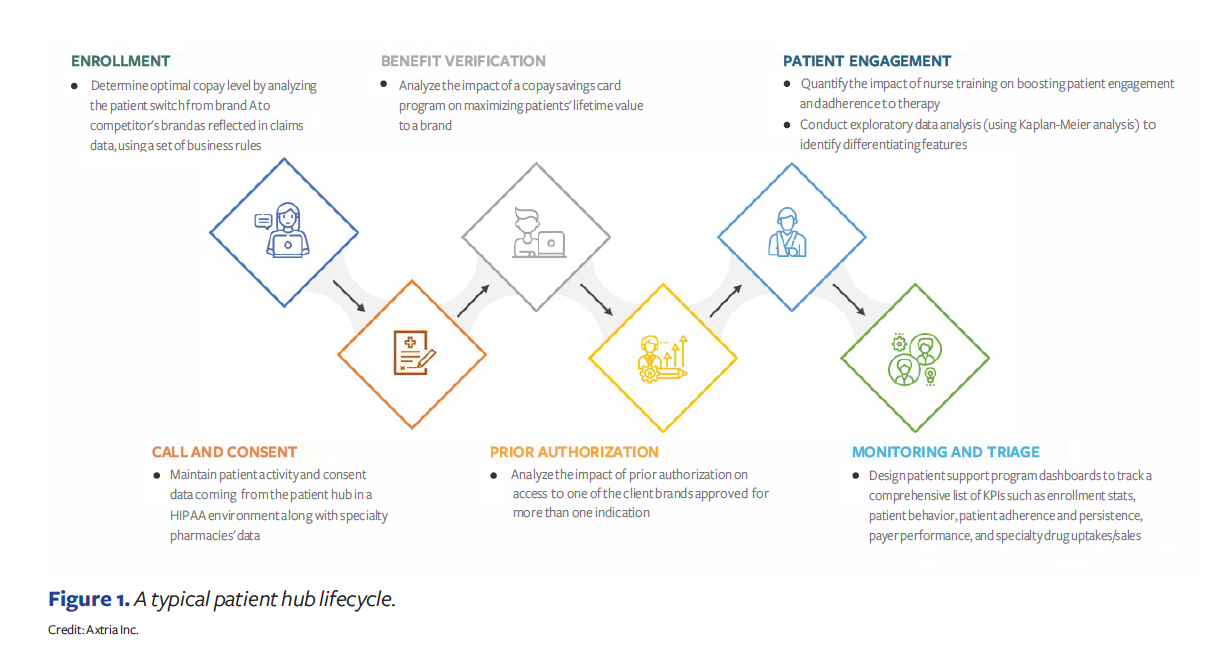
When patient hubs started in the 1990s, they provided minimal services, such as helping patients and providers with the complex reimbursement process for specialty medications and collecting data related to these services. Today, they have evolved to offer and manage a whole suite of data and services related to consent management, benefits verification, prior authorization, drug delivery, administrative support, copay, financial assistance, disease awareness and education, monitoring and triaging, patient reporting, and any risk evaluation and mitigation strategy (REMS) program management. Even though the range of services provided by today’s hubs is much more comprehensive, patients may still find them a bit difficult to use. A recent Bain & Company survey showed that 53% of patients felt pharma companies need to provide two things: more targeted patient support programs and a single source of content.
The modern patient hub
Although different models are evolving, manufacturers have traditionally outsourced the management of their hubs to a hub provider. Now, with the advent of specialty drugs like CAR-T and gene therapies across oncology, rare diseases, and others, manufacturers are insourcing disease-based, specialized skills, while outsourcing logistical tasks. The current focus is on designing programs specific to individual therapeutic areas. However, these programs have yet to provide the expected benefits to the patients they were intended to help.
Patient hubs depend on the fundamental assumption that data, technology, and people will come together seamlessly to provide the right interventions across the right channels at the right time, in order to create a pleasant omnichannel experience for the patient in an empathetic manner, rather than sympathetic.
Many issues are due to process and integration problems at the hub level, causing downstream impacts for the patient. That prevents hubs from fulfilling the promise of enhanced patient engagement.
The underlying data issues
Downstream commercial systems depend on integrating various data sources, including the tokenized patient hub and specialty pharmacy data, that makes it possible to run analytics. The quality and correctness of that information is important at all stages of the patient journey. For example, case managers capture a lot of data during enrollment, at initiation, during therapy, and after discontinuation. They play a crucial role by updating the details of follow-ups, services, and case statuses in hub applications. Any gaps in the data capture can limit the value of analytics with respect to costs, coverage, treatment options, and access to the drug and adherence.
Vishal Singal

Pharma companies have a host of data sources, yet they still depend on hub data to get a good view of a patient’s journey and ensure they deliver actionable insights into specialty drug programs. Many hub providers have varying degrees of capability and support when integrating data and providing analytics. In addition, consent management plays a role, as permission requirements can be obtained across hubs and specialty pharmacies. It is imperative to manage this process efficiently, so that individual patients can be reached across channels, such as calls, text, email, digital, and traditional mail for any type of intervention.
The next step in patient engagement
In the future, to enable better engagement throughout the journey—from prescription to therapy initiation to adherence—there must be more flexibility when addressing patient needs beyond the clinical factors. For this to happen, we must focus on finding and understanding the right patient cohorts at a therapeutic and drug-specific need level. Then, the clinical and non-clinical data at all points must be integrated. That will optimize the reach, frequency, and sequence in an omnichannel environment to drive patient engagement and outcomes.
Patient hubs must go beyond the current methods of reaching
out to drive patient engagement, but they need not focus on a “revolution.” Instead, they should look toward “evolution,” where processes around consent management, benefits verification, prior authorization, triaging, and therapy dispensation are simplified. The process should be flexible and easily adaptable to unique patient populations. Take, for example, an elderly patient who lives alone and has some comorbidities. When prescribed a new injectable cardiovascular drug, this patient may need more human-based, personalized engagement in his or her treatment plan. However, another segment of elderly patients on the same drug, but with a support structure of younger caregivers, might be open to digital interventions. Understanding the subtle differences in patient cohorts is the key to driving more engagement. Case managers, reimbursement specialists, copay administrators, and others supporting the hub must be empathetic to patient needs. They need to be able to imagine themselves in a similar circumstance and develop a deeper knowledge of their specific therapy area so they can help assuage any patient concerns about drug efficacy and the disease itself. Further, hubs should also be able to reduce process complexity by helping each patient cohort understand the existing guidelines, pathways, and other decision-support frameworks.
Integrating the right data
Nalini Somavarapu

Data is the key to resolving issues across the patient journey, but its quality, granularity, access, and timeliness present challenges in hubs. Data is becoming even more complex and is spread across multiple systems, especially now with the rise of new classes of therapeutics, such as gene therapies and CAR-T. A gap in any of the data pipelines can have a great deal of impact on downstream analytics. Providers play an essential role in ensuring patients use prescribed therapies correctly and consistently. Timely and granular data on the payer’s and patient’s cost for the drug makes it possible for care teams to intervene at the right time, reducing barriers to affordability and access, and enhancing patient engagement. Better integration between provider offices and hubs can help resolve problems expeditiously, and reduce data and administrative issues. Tracking hub performance and issues related to patient engagement can go a long way in plugging the data gaps and streamlining the overall process.
Pharma manufacturers would also like to integrate all data into the hub and access it in near real-time. That allows them to monitor performance and work collaboratively with the hubs to troubleshoot any issues. Data aggregation is arguably the most critical aspect of downstream analytics because it links all data sources, from the hub to the specialty pharmacy to the copay. Understanding the appropriate usage of personally identifiable information is vital to avoiding compliance issues and helping resolve other problems along the patient journey.
One of the biggest hurdles hubs face is getting patients started on a treatment. Fast Start and Bridge are examples of programs that provide free goods before a wider dispense begins. Hubs or pharmacies have the authority to enable these services, based on the availability of high-quality data, to ensure that patients have a seamless introduction to their therapies.
Optimizing the engagement
Patient engagement takes place across various touchpoints, programs, and channels. Optimizing the reach by customizing the frequency, sequence, and recency of these interactions, vis-à-vis therapeutic area and patient cohorts, is important from the patient engagement perspective. Let’s look at two examples of how small changes in interactions can produce significant increases in patient engagement:
- A recent Axtria analysis of patient support programs for a client in the cardiovascular therapeutic area found that by following patient-nurse interactions with savings card information, a 2% increase in the overall duration of therapy for that drug was achieved. In contrast, the combination of peer-to-peer conversation followed by nurse interaction generated a 5% increase in the patients’ overall duration of therapy.
- In another Axtria analysis for a rare cardiovascular drug, a targeted approach to identifying high-risk patients, followed by adjusting the frequency of nurse interventions, improved the overall duration of therapy by 30 days.
In one of those examples, getting the desired results depended on adjusting the program sequence. In another, a targeted approach of identifying high-risk patients, then focusing on the frequency of reach, was effective at improving drug adherence.
Although both examples happened in a similar therapeutic area, the approach to patient engagement was different. With so many different classes of treatment today, patients are demanding a deeper level of personalization along their journey in an omnichannel environment. Many interventions are through a nurse navigator, reimbursement specialist, digital reminder, disease awareness content, or other forms across digital and non-digital channels. With this rising complexity, it becomes more important to understand that it takes a combination of channels and interventions, in the right order, to get patients started and remain on a therapy.
More investments will be needed, including a focus on hiring nurses trained in specific therapeutic areas, making data integration with provider offices a priority, investing in physician and patient education, developing customer-friendly digital tools, and simplifying processes to enhance the experience and help pharma companies with their new product commercialization.
About the Authors
Vishal Singal is Patient Engagement and Digital Health Lead; Nalini Somavarapu is Senior Manager, BIM; both at Axtria.