Accelerating the drive toward patient centricity
Getting away from the traditional product-centric management structure is not easy; here’s how to do it

Consumers have grown accustomed to on-demand services, whether it’s Amazon recommending your next favorite television series to binge-watch or Uber arriving at your doorstep the moment you need to depart for the evening. With health tech startups offering virtual doctor visits through your phone (like on-demand healthcare service 98point6) and leveraging virtual reality to deliver pain relief, consumers are starting to expect the same from their healthcare experiences.
Historically, the pharmaceutical industry has been slow to respond to changing market dynamics. Companies could afford to take a more plodding, conservative approach given that the industry used to be largely product-centric. But times are changing, and consumers are becoming accustomed to a more frictionless, patient-centric healthcare experience, whether it’s booking a ride-share to visit the doctor or making an appointment through ZocDoc. If the pharmaceutical industry intends to stay relevant, there’s a dire need to shift the mindset and culture of the industry away from product centricity and toward patient centricity.
The good news is that many large pharmaceutical companies have received the message and have already started to make investments to shift their organizational mindset. The not-so-great news is that patient centricity efforts can appear disjointed and feel, at times, like corporate window dressing. We believe that for the industry to evolve, the patient-centric movement must transcend individual corporate efforts. It must be a collaborative approach among internal experts and knit together disparate investments and initiatives.
To that end, after conducting extensive research, interviews, and analysis of the industry and discussing the issue with a group of industry experts as part of ZS’s Patient Centricity Advisory Board, we’ve put together three guidelines that will help guide pharma companies explore the brave new world of patient centricity.
1. Patient centricity is change management. Embracing patient centricity shouldn’t be thought of as distinct from change management. Patient centricity is change management. The patient-centric model should be relevant across the entire organization with a shared purpose and mission. When organizations commit to shifting from product centricity to patient centricity, it’s essential that their efforts go beyond corporate communications and are engrained in the operations of every department.
Change initiatives have produced a wide array of patient centricity models—ranging from grassroots to federated models—yet no single model has proven to be the perfect choice. Nevertheless, one theme that has consistently emerged is that for change to stick, there’s a need for a dedicated and resourced group to advocate, train and accelerate patient centricity efforts across the organization. By identifying and scaling a team of internal facilitators who are trained in applied empathy and human-centered design, the company can democratize patient centricity practices and capabilities. Eventually, those who are trained will form the backbone of an enterprise-wide network of patient centricity advocates. Change is hard, and the most successful change management initiatives rest upon the commitment of a centralized team with subject matter expertise.
It’s hard to accurately measure patient centricity. Why? The definition of “patient centricity” varies based on which function you serve inside of your organization. Nevertheless, having meaningful measures across the enterprise is essential to the sustainability of your patient-centric efforts, and the metrics need to follow each touch point of the patient experience. Measurement should begin in clinical research and continue through the entire product life cycle, touching nearly every part of the business.
If you are thinking about trust and reputation as key by-products of successful patient-centric efforts, you can look to Net Promoter Scores (NPS) and reputational surveys, but it’s equally important to consider clinical measures such as a patient’s treatment adherence and feedback on the product experience. Additionally, we need to be careful choosing metrics that aren’t predictive of long-term patient value. It’s often the case that too much emphasis is placed on patient metrics that the investment community deems important—for example, the race to get to “first patient/first dose” in clinical trials—yet these metrics have limited patient value.
3. Cross-industry collaboration is the new competitive advantage. The pharmaceutical industry has traditionally been a highly competitive industry where proprietary know-how is essential to maintain a competitive advantage. However, research indicates that while there are some industry leaders in patient centricity, no one organization has figured it out, especially when compared to those providing first-rate customer-centric experiences within other industries. To that end, it’s essential to build an ecosystem with various stakeholders. Working together as an industry and sharing insights can lead to collective, industry-wide benefits. By periodically collaborating across the industry and using universally upheld and validated benchmarks, organizations can continually assess their patient-centric portfolio of investments. A regular model of engagement with intra-industry partners is the rising tide that lifts all boats.
Connecting with patients within legal parameters
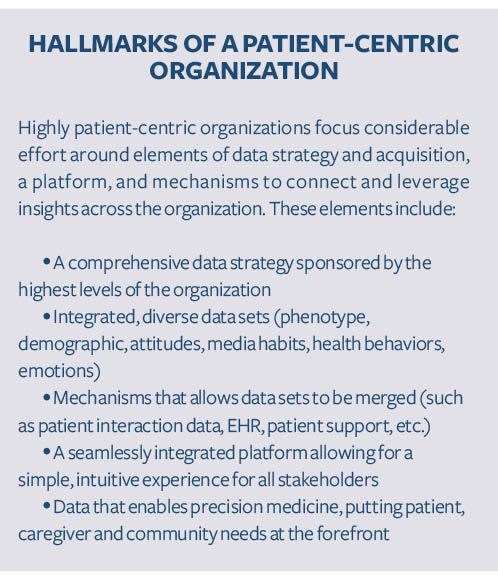
Patient insights and data play a key role in supporting organizations as they approach patient centricity. Key questions often arise about the types of data and insights that may be gathered. There’s also considerable confusion in the industry about pharma companies’ access and right to access patient information. While access is largely dictated by patient permissions, here are some opportunities for pharma companies to connect with patients while being mindful of their personal information:
1. Primary market research: Pharma researchers can gather patient information while following guidelines set forth by industry organizations like EphMRA, BHBIA or Insights Association. By assuring that individually identifiable information is protected, adverse events are reported, and regional laws such as GDPR are followed where they apply, we can conduct market research with patients and remain compliant. The type of information that may be collected and that can be shared with the pharma company will vary by country.
2. Ongoing, contractual engagements: Pharma companies can create patient panels or advisory boards to gain input for decisions and materials. The involved patients sign a contract that includes straightforward regulatory guidelines, and pharma companies can use their input for designing clinical trial protocols, patient support programs, and messaging and marketing materials, or to investigate HCP and patient interactions. The type of information that may be collected from the patients, how it will be used and by whom will be detailed in the contract. Typically, the function sponsoring the advisory board will have some level of access to some level of patient information as detailed in the contract.
3. Patient support programs: Patients opt-in for support and communications from pharma, which can include things like information about their condition or prescription, medication reminders, co-pay cards, nurse support, or other relevant content. During the opt-in process, the patient gives permissions that determine the information you can collect from them. The internal patient support function at a pharma company and an analytics team would typically have access to de-identified information, often at an aggregate level to ensure that privacy is not compromised.
4. Registries: This allows pharma companies to enlist a third-party company to build and maintain a registry that collects patient information over time. Pharma sponsors would have access to certain parts of this data.
Exploring and utilizing patient data and insights are critical to becoming a truly patient-centric organization. Only through understanding patients—and their needs and experiences—can pharma seek to orient around the patient in a way that makes sense for its business. Navigating regulations and compliance around patient data may seem daunting, but companies that can effectively overcome this hurdle can gain great insight and a competitive advantage.
Change in the pharmaceutical industry is inevitable. Consumer-led innovation has disrupted many industries, and pharma is next on the change management chopping block. Investing in a patient-centric culture and capabilities will go a long way in resetting how the industry and individual companies operate.
About The Authors

Sharon Suchotliff is a manager in ZS’s New York office. She has 15 years of marketing communications experience across a broad range of categories, from fashion and lifestyle to pharma and healthcare. At ZS, she focuses on patient centricity and helping organizations incorporate the patient voice in development through commercialization, in ways that make sense for their business.

Hensley Evans is a principal in ZS’s Zurich office and is the leader of ZS’s Patient and Consumer Health practice. Hensley has worked with many of the world’s top healthcare, biopharmaceutical and consumer packaged goods brands to offer strategic direction and insight.
Newron, Myung In Pharm Form Partnership Centered Around Treating Schizophrenia in South Korea
January 14th 2025The license agreement will feature an upcoming Phase III trial and—depending on results—the development, manufacturing, and commercialization of evenamide as a potential treatment option.